Abstract
Metabolic rewiring, a hallmark of acute myeloid leukemia (AML), contributes to the development of resistance to intensive chemotherapy and has been shown to play an essential role in leukemic cell maintenance. Several metabolic alterations have been described in AML, such as dependence on amino acids to fuel oxidative phosphorylation or ability of leukemic cells to switch energy dependence to fatty acid oxidation in response to treatment. However, little is known about the functional significance of the fatty acid synthesis (FAS) pathway in AML.
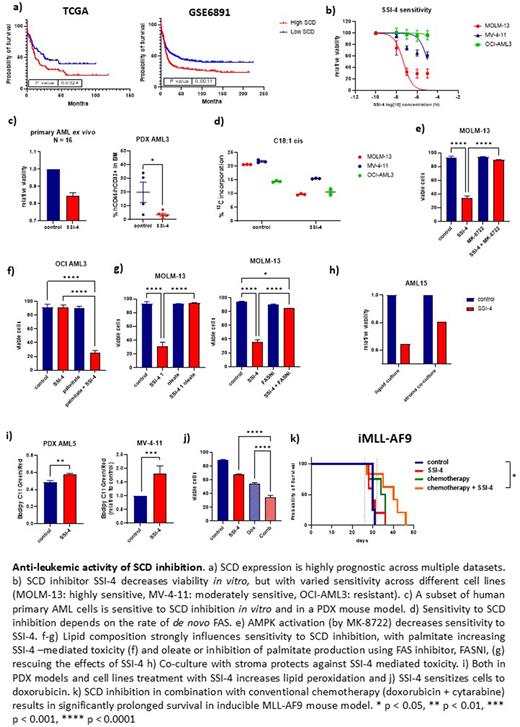
Here we have identified stearoyl-CoA desaturase (SCD), a key enzyme responsible for the conversion of saturated fatty acids (SFA) into monounsaturated fatty acids (MUFA), as a novel therapeutic target in AML. High SCD expression predicts worse survival across several patient datasets, even after correction for gender, age and AML European LeukemiaNet risk category. Moreover, genetic and chemical inhibition of SCD reduces growth and induces cell death in AML cells. Since targeting SCD with currently available inhibitors has been challenging because of their toxicity profile in vivo, we have accessed a novel pharmacological SCD inhibitor with a more favorable toxicity profile, SSI-4 (Modulation Therapeutics Inc., Morgantown, USA). SSI-4 reduces viability in several human and mouse AML models in vitro and in about half of the 36 primary AML samples tested ex vivo. Moreover, SSI-4 displays anti-leukemic effects in AML murine models and patient-derived xenografts (PDX).
Since we could not correlate susceptibility to SCD inhibition with any genetic characteristic of AML cells, we aimed to determine the molecular basis of cell sensitivity using phosphoproteomic, proteomic and transcriptomic approaches coupled with metabolic analyses of sensitive and resistant cell lines and primary AML cells. Sensitivity to SCD inhibition directly correlates with rate of de novo FAS, as measured by fatty acid labeling with 13C-glucose. Moreover, modulation of FAS by the AMPK signaling activity dictates sensitivity to SCD inhibition and AMPK activation rescues the anti-leukemic effects of SSI-4.
The anti-leukemic effects of SCD inhibition are secondary to the induction of SFA mediated lipotoxicity, as demonstrated by the increased sensitivity of previously resistant cells to SSI-4, when grown in the presence of the SFA palmitate. Conversely, growing cells in the presence of the MUFA oleate, as well as inhibition of FAS by targeting enzymes upstream of SCD, results in resistance to SSI-4, thus confirming that the increased SFA/MUFA ratio drives leukemic cell death. SFA mediated lipotoxicity leads to both increased lipid peroxidation and activation of the unfolded protein response (UPR), namely its PERK branch, which in turn leads to apoptotic cell death. Indeed, inhibition of PERK, but not of other branches of UPR, rescues SCD-mediated cytotoxicity.
Despite causing disease debulking in vivo, SSI-4 does not prolong survival in murine AML models as a single agent and the toxic effects of SSI-4 are decreased when AML cells are grown in co-culture with stroma, suggesting a protective role of tumor microenvironment. However, we consistently detect increased lipid peroxidation and DNA damage both in vitro and in vivo following SCD inhibition. We therefore combined SSI-4 with doxorubicin, a known inducer of lipid peroxidation and DNA damage, which is routinely used in AML induction therapy. Indeed, both genetic depletion and pharmacological inhibition of SCD renders AML cells more sensitive to doxorubicin, and addition of SSI-4 to a standard AML chemotherapy protocol consisting of doxorubicin and cytarabine significantly extends survival in AML mouse models.
In summary, we identify and validate SCD as a therapeutic target in AML. The novel SCD inhibitor SSI-4 displays anti-leukemic properties both in vitro and in vivo across different AML models and particularly when combined with standard chemotherapy while showing minimal toxicity in vivo. We show that sensitivity to SCD inhibition is driven by metabolic rather than genetic AML features, thus making this therapeutic approach potentially applicable across several AML subtypes, including high risk ones. Finally, the mechanism of toxicity following SCD inhibition suggests that this can be further enhanced by modulating the levels of SFA/MUFA through dietary interventions or by combining it with DNA damaging agents.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.